A Letter from Dr. Ron Korstanje of ASF’s Scientific Advisory Research Network
Everyone has a unique genetic background that affects how we look, how we behave, and how diseases develop. This is, in part, why patients with Alport syndrome (AS) who have similar variants in their collagen genes can have differences in disease development and progression.
The Korstanje lab at The Jackson Laboratory in Bar Harbor, Maine (www.jax.org/korstanje-lab) is interested in identifying the genes that play a role in these differences (so-called modifier genes), as these can be potential targets for therapies to slow disease progression.
Since this is difficult to do with human patients, we use an approach in mice that mimics a human patient population. We have taken a mouse model with a Col4A5 mutation (developed by Dr. Michelle Rheault, of ASF’s Medical Advisory Committee) and crossed this with genetically diverse mice. This resulted in a cohort of mice where each mouse has a unique genetic background (like a human population), while also having the Col4A5 mutation. In this cohort, there is a large variation in the age of onset and severity of kidney disease (like a group of human patients) and allows us to identify which genes are responsible for these differences.
We first tested this approach on a cohort of 100 male mice and 100 female mice and identified several modifier genes (Takemon et al, 2021) that we are now studying for their role in the disease. We are also testing several drugs based on these genes. However, there were hints of more modifier genes, but our cohort of 200 mice was not large enough to be sure. We have now made a second cohort increasing the cohort with another 200 males and 200 females and have measured kidney function and kidney damage in all these animals. We will soon be able to do the genetic analysis on this large cohort and expect to identify additional modifier genes.
During the 2021 International Workshop on Alport Syndrome, there was a discussion about some patients with AS having renal cysts and what could be driving this pathology. This prompted us to look at the kidneys that we collected from our first cohort of mice, and we quickly found that some of our mice, like the human patients, have renal cysts. This means that the presence of renal cysts in AS must be genetically driven and that it should be possible to identify the causal genes. Identifying these genes will lead to a better understanding of the disease process, which can result in better diagnosis and treatment. (To read more about the presence of cysts in Alport patients, please see the article links at the bottom of this page.)
Looking for renal cysts in 600 kidneys is a lot of work. To help us with our first cohort (200 mice), we digitized our microscope slides and posted them online. In 2022, we asked volunteers from the Alport community to look at the slides and give each a score between 0 and 2 (0 = no cysts, 1 = some cysts, 2 = many cysts). When we analyzed the data that was collected by the volunteers and we combined this with our albuminuria data from the mice, we found a strong correlation (see figure below).
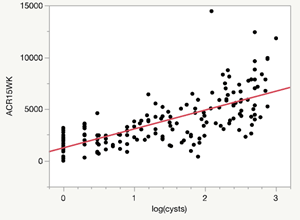
Unfortunately, scoring 200 kidneys was not enough to find specific genes in the genetic analysis (there were some hints, but not strong enough to be sure). Now that we’ve added an additional 400 kidneys for analysis, we believe this will be enough to find the responsible genes once the kidneys are scored.
Read More
To make this possible, we need your help. There are about 360 slides to be evaluated at this time. And you do not have to be concerned about making mistakes – the power will be in the number of people who volunteer. If many people score small groups of kidneys, there will be overlap. In this way, all kidneys will be scored multiple times and by averaging the scores for each kidney, we will dilute errors.
1
How to Access the Slides
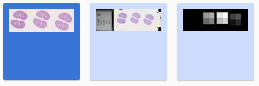
If you are willing to help us, please go to our online kidney collection, where you will find images of all kidneys from the new cohort. There are three images for each kidney, but it is the first image with the name ending with ‘[0]’ (as see in top right of screen) that you want to open by double-clicking on the slide or the name in the left hand column.
See the dark blue image below and on the left as an example of which image within a set of three that you will be analyzing:
This comes out to about 360 kidney slides in total to review.
There are three sets of kidney shapes on each slide file ending in [0], but you only need to score one (it should not matter which one). Some sections do not show a complete kidney (something went wrong with cutting the tissue) and you want to skip those images.
The easiest magnification for slide assessment is also the smallest (2.5x). You can see which magnification you are looking at on the bottom left of the image screen. Continually click the minus sign “-” located below the “+” and “1:1” in the top left-hand corner of the image to reduce magnification down to 2.5x. You can move the section by dragging the mouse while keeping the right button pressed (or keeping the trackpad pressed on a Mac).
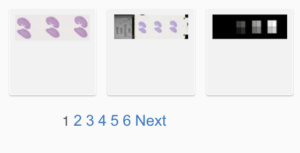
Please note that there are multiple pages of slides to review (6 pages total). Once you have finished scoring all of the slides on the first page, you will see blue numbers at the bottom of the screen, indicating which page you are on. To advance to the next page, simply click the blue “Next” (as shown below).
2
How to Identify Cysts
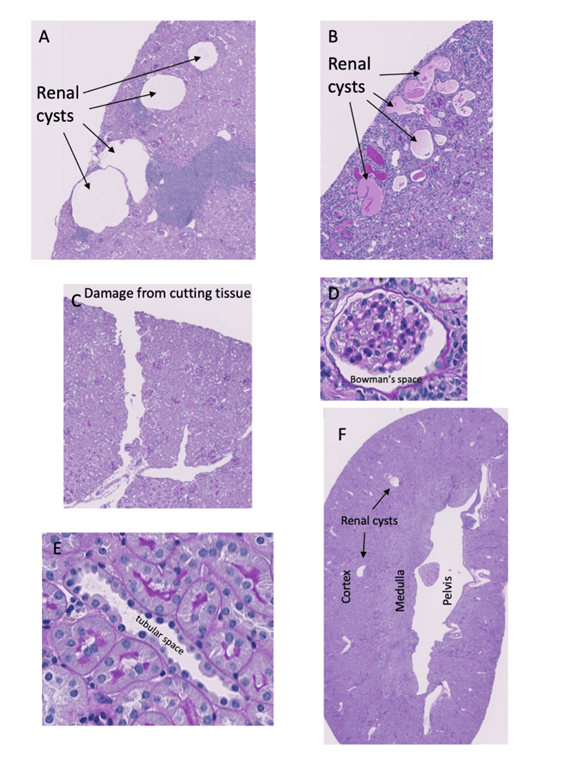
Below the following descriptions, there are images labeled A to F that illustrate what cysts do and do not look like.
Cysts will appear as spaces in the kidney that have smooth edges and look like bubbles that could have been caused by the pressure of liquid buildup (A).
They are sometimes filled with a purple substance (B), which is protein. This contrasts with some of the white spaces that you may see that were caused by the tearing of the tissue during the process of cutting the kidneys to make the slides (C). Those are more irregular and don’t have smooth edges.
Other small white spaces in the kidney that you may find, but are not renal cysts, are (D) around glomeruli (called the Bowman’s space) and (E) tubular space. There is a higher chance of finding white spaces that are NOT cysts in the medulla and the renal pelvis (closer to the middle of the kidney), compared to the cortex (around the edges of the kidney) (F), so focus on the cortex.
Again, don’t worry too much about making a mistake every now and then. We expect everyone to make some mistakes, but because different people will make different mistakes, they will average out.
3
How to Record Your Results
Email ASF’s Associate Director Afton DeLucca at [email protected] to receive your “Cyst Scoring Sheet”. On this sheet, you’ll see the animal number in the first column, which corresponds to the number in the image file name ending in [0] that you viewed. You’ll record your numeric score next to each animal number in the “Cyst Severity 0-2” column.
If you are unable to score all of the slides, that is perfectly fine! In this case, please choose a random starting point (mouse number) on the scoring sheet and proceed from there. That way, all of the images will be scored by multiple people, improving the overall scoring accuracy.
When viewing the slide at 2.5x magnification, you can always double check the image file name by clicking “Image Information” located on the left-hand side of the screen.
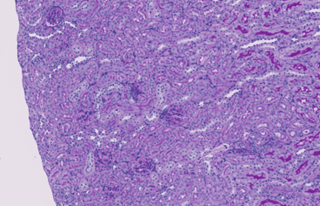
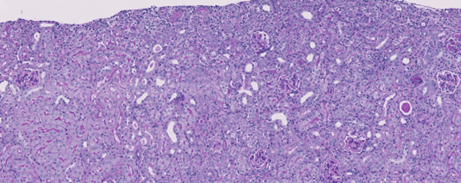
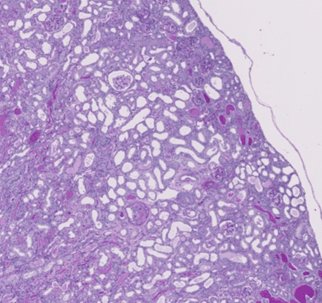
Please see the reference images below, which show examples of each score (0-2):
Score = 0
Score = 1
Score = 2
4
How to Submit Your Completed Scores
Once you have analyzed and scored all of the slides, save the scoring sheet with your initials at the end of the file name. Please email your completed spreadsheet to Ron Korstanje ([email protected]) and copy ASF’s Associate Director Afton DeLucca ([email protected]). Please submit all scoring sheets no later than June 30, 2024.
Kindly indicate in your email whether you would like to stay informed of the results and be contacted again to help with future studies.
Further Reading
Kidney Cysts in Children with Alport Syndrome: a Report of Three Cases
Chang, Yeun-Wen et al.
Kidney Medicine, March 25, 2024.
Clinical Significance of the Cystic Phenotype in Alport Syndrome
Zeni, Letizia et al.
American Journal of Kidney Diseases, March 19, 2024.
Cystic phenotype and chronic kidney disease in autosomal dominant Alport syndrome
Bada-Bosch, Teresa et al.
Nephrology Dialysis Transplantation, January 4, 2024.
Alport Syndrome With Kidney Cysts Is Still Alport Syndrome
Savige, Judy et al.
Kidney International Reports, November 9, 2021.